Bulimia
Bulimia nervosa: symptoms, causes and treatment
Bulimia can manifest through a variety of different bingeing and purging patterns. Individuals may have powerful urges to overeat and this is then followed by periods of starvation or food restriction. They may fast, skip meals, follow strict diets or eliminate certain food groups from their diet. Some people may then purge or vomit as a strategy for managing their weight.
Some people suffering from bulimia never force vomiting at all. That’s because the concept of bulimia nervosa has to do with a pattern of bingeing and purging or starving, not just vomiting specifically.
There are two types of bingeing behaviours:
Subjective Bingeing
Objective Bingeing
The difference between Bulimia and Binge-eating disorder is:
The difference between Bulimia (non-purging) and Binge-eating disorder is the behaviour that happens after a binge.
• Bulimia (non-purging)
• Binge-eating disorder
Types of Bulimia
- Self-Induced Vomiting
- Misuse of Laxatives
- Misuse of Diuretics
- Misuse of Enemas
The non-purging type of bulimia is still equally problematic and dangerous. In this case, the patient will go to other excessive measures in the wake of their binge. They may:
- Fast Excessively (Self-Starvation)
- Exercise Excessively
What causes of bulimia?
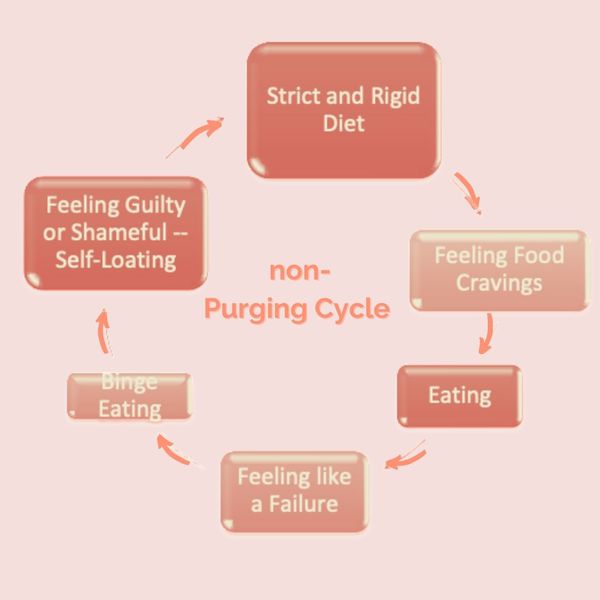
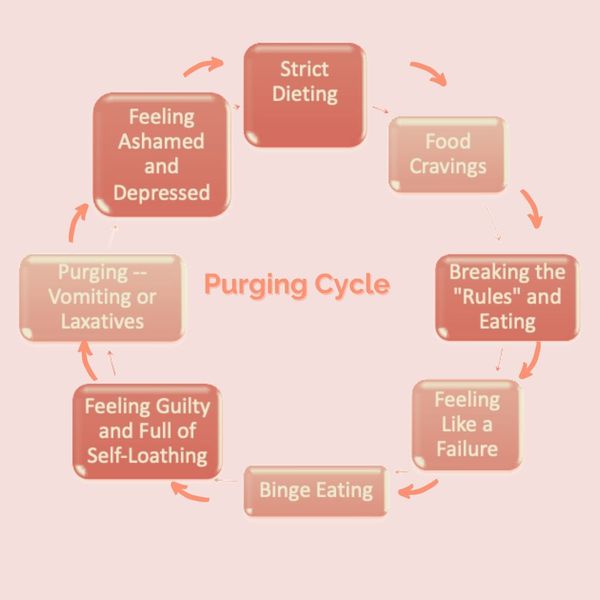
These diagrams illustrate the vicious circle of bulimia and show how these eating patterns become reinforced. Thus, strict dieting often leads to food cravings, following by eating something, then feeling like a failure, leading to a binge, after which feelings of guilt and self-loathing emerge. Purging would then occur to relieve these feelings, however, following a purge, even further uncomfortable feelings develop. And so the cycle continues.
The following example is of a non-purging bulimic cycle, following similar patterns.
The fact that bulimia tends to run in families also suggests that a susceptibility to the disorder might be inherited.
Impact of Bulimia on Individuals
Physical Impact of Bulimia
- Fatigue, muscle weakness, dizziness, and fainting due to an imbalance in electrolytes.
- For women, missed menstruation and even long-term or permanent infertility
- Loss of blood flow leading to anaemia and starvation of organs.
- Cardiovascular (heart) damage including arrhythmias, heart disease, and high cholesterol.
- Loss of vitamins and minerals leading to a compromised immune system.
- Tooth decay and oesophageal tears and bleeding from vomiting
- Dehydration and gastrointestinal distress from chronic use of laxatives.
- Kidney damage or failure.
- Loss of bone leading to long term osteoporosis.
- Retarded growth and thyroid malfunction in youths.
- Long-term bulimia could lead to organ failure, including heart failure, and can be fatal.
Psychological Impact of Bulimia
- Stress or difficulty in food related situations.
- Self-imposed isolation and refusal to develop relationships.
- Constant fear of disapproval from others.
- Mood swings, strong emotions, and depression.
- Suicidal thoughts, tendencies, or attempts.
- Overwhelming feelings of guilt and self-loathing.
- Development of anxiety disorders.
Impact of Bulimia on Family and Friends
What is the treatment for bulimia?
Guided self-help
Cognitive behavioural therapy (CBT)
How is treatment designed for each individual?
Changes in relationships with food and body image change during treatment
What would be the signs that someone has overcome bulimia?
References:
Fairburn, C. G. (2008). Cognitive behavior therapy and eating disorders. New York, NY: Guilford.
Gowers SG. “Management of Eating Disorders in Children and Adolescents,” Archives of Disease in Childhood (April 2008): Vol. 93, No. 4, pp. 331–34.
Herzog D, et al. Unlocking the Mysteries of Eating Disorders: A Life-Saving Guide to Your Child’s Treatment and Recovery (McGraw-Hill, 2008).
Juarascio, A., Lantz, E. L., Muratore, A. F., & Lowe, M. R. (2018). Addressing weight suppression to improve treatment outcome for bulimia nervosa. Cognitive and behavioral practice, 25(3), 391-401.
Lowe, M. R., Piers, A. D., & Benson, L. (2018). Weight suppression in eating disorders: a research and conceptual update. Current psychiatry reports, 20(10), 80.
Le Grange D, et al. “Predictors and Moderators of Outcome in Family-Based Treatment for Adolescent Bulimia Nervosa,” Journal of the American Academy of Child and Adolescent Psychiatry (April 2008): Vol. 47, No. 4, pp. 464–70.
Shapiro JR, et al. “Bulimia Nervosa Treatment: A Systematic Review of Randomized Controlled Trials,” International Journal of Eating Disorders (May 2007): Vol. 40, No. 4, pp. 321–36.
Williams PM, et al. “Treating Eating Disorders in Primary Care,” American Family Physician(Jan. 15, 2008): Vol. 77, No. 2, pp. 187–95.